The Connection Between Substance Abuse and Suicide
Written By
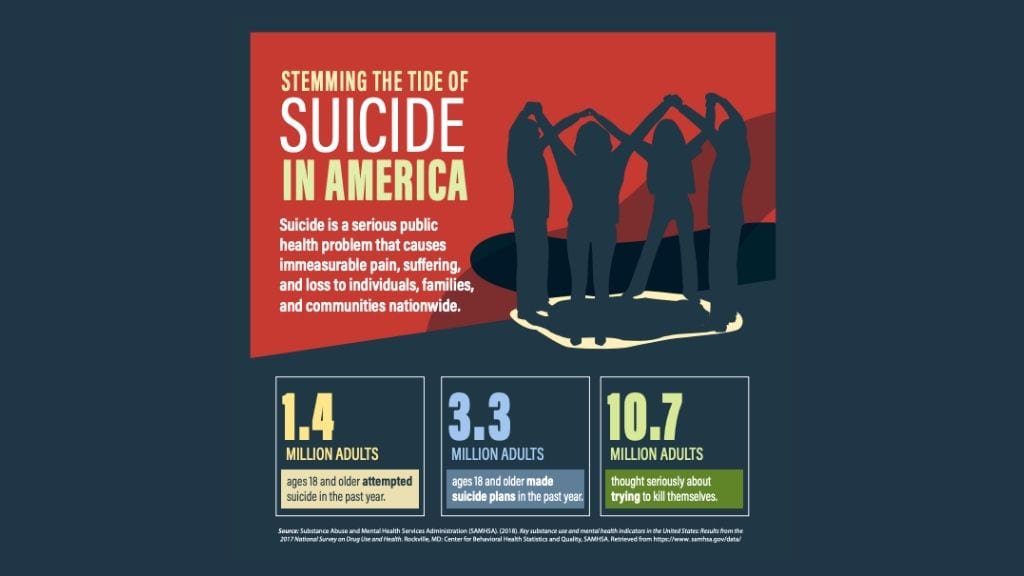
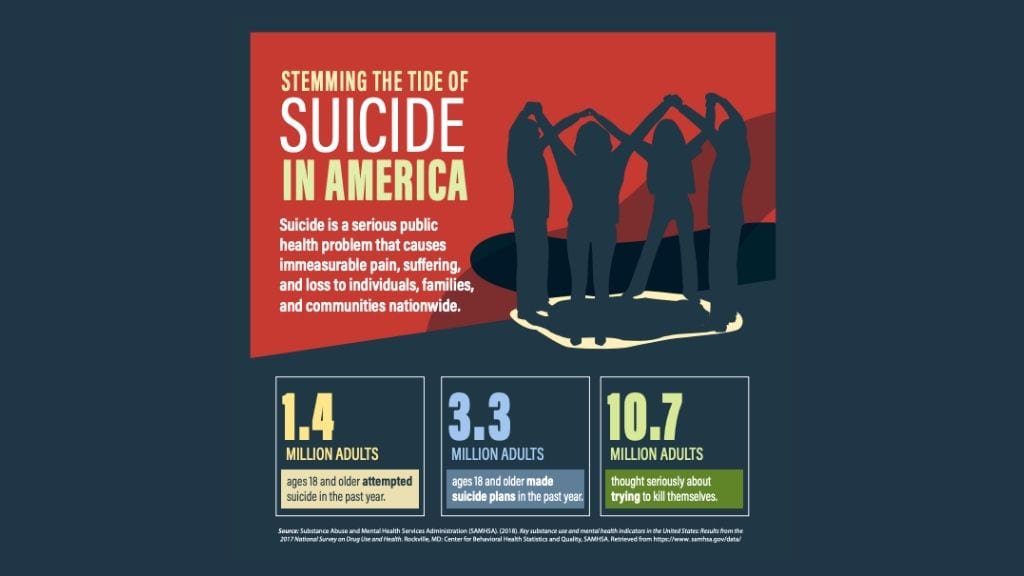
DreamLife RecoveryChances are you, or someone you know, has been touched by the tragedy of suicide. With suicide rates increasing at a dramatic clip, gaining a deeper understanding of the impact of substance abuse on mental health, and how it can increase the risk of suicide, is appropriate during SAMHSA’s National Prevention Week.
How Does Substance Abuse Contribute to Suicide Rates?

One of the leading risk factors for suicide is substance abuse. Addiction to alcohol or drugs often coexists with a mood disorder, such as depression, anxiety disorder, or bipolar disorder. The co-occurring disorders evolve in one of two ways: 1) with the effects of the mental health issue fueling substance abuse, or 2) with the effects of addiction causing psychological distress. Whichever way the dual diagnosis evolves, the risk for suicide is significantly increased.
Men with co-occurring alcohol use disorder and depression have the highest long-term suicide risk, at 16.2%. The prevalence of lifetime suicide attempts among individuals with co-occurring alcohol use disorder and bipolar is somewhere between 21%-42%, according to a study published in The American Journal of Psychiatry.
But the connection between substance abuse and suicide does not necessarily have to include a comorbid mental health disorder. In fact, those with alcohol dependency have a ten-times higher risk of suicide, and individuals who abuse drugs have a 14-times greater risk of suicide, regardless of the existence of a mental health disorder. This may be explained by certain personality traits and lifestyle habits that are common among people who abuse drugs and alcohol, such as impulsivity, poor judgment, and engaging in high-risk behaviors. The negative consequences of a substance use disorder, including damage to relationships, loss of employment and financial distress, health problems, and homelessness also factor in to the effects of substance abuse on suicidality.
When suicide postmortems are conducted, it is discovered that more than a third of the victims of suicide had alcohol in their bloodstream. In fact, approximately one in three were under the influence of drugs or alcohol at the time of the suicide. The chart below shows the number of individuals with various substances present in their systems after completing suicide in 2013.
Suicide Warning Signs
 According to the American Foundation for Suicide Prevention (ASPS), more than 47,000 Americans died last year by suicide. ASPS reminds us that for every completed suicide, there are about twenty-five attempted.
According to the American Foundation for Suicide Prevention (ASPS), more than 47,000 Americans died last year by suicide. ASPS reminds us that for every completed suicide, there are about twenty-five attempted.
The warning signs include:
- Say they are a burden to others
- Talk about feeling hopeless, or have no reason to live anymore
- May be acquiring the means to commit suicide, such as buying a gun or stockpiling drugs
- Mention wanting to die, or that they are considering suicide
- Excessive sleeping or insomnia
- Isolating behaviors, withdrawing socially
- Increased use of alcohol or drugs
- Behaving recklessly
- Agitated or anxious
- Saying they feel trapped in their pain
- Mood swings
- Giving things away that have special meaning
Alcohol Abuse and Suicide
 According to a clinical study [Beck, Steer], alcoholics have a five times greater risk of committing suicide than non-alcoholics, regardless of whether there is a co-occurring mental health disorder. Alcohol is a depressant, and when combined with negative life events can trigger feelings of despondency and hopelessness. Individuals under the influence of alcohol are not able to keep perspective or think clearly about their options, and may indulge in impulsive or risky activities, including attempting or completing suicide.
According to a clinical study [Beck, Steer], alcoholics have a five times greater risk of committing suicide than non-alcoholics, regardless of whether there is a co-occurring mental health disorder. Alcohol is a depressant, and when combined with negative life events can trigger feelings of despondency and hopelessness. Individuals under the influence of alcohol are not able to keep perspective or think clearly about their options, and may indulge in impulsive or risky activities, including attempting or completing suicide.
Benzodiazepine Abuse and Suicide
 A recent study [Dodds] found that the use of benzodiazepines (sedatives) and hypnotics (sleeping pills) is associated with a three-fold higher risk of suicide attempts. These drugs are prescribed to those who struggle with anxiety disorders or insomnia and are highly addictive due to rapidly increased tolerance. While the possibility exists that the insomnia and anxiety are to blame for the suicidal behaviors, several other studies seem to suggest that the drugs themselves were causing the suicide attempts. In addition, these sedatives are often used as a tool to complete a suicide, often combined with alcohol.
A recent study [Dodds] found that the use of benzodiazepines (sedatives) and hypnotics (sleeping pills) is associated with a three-fold higher risk of suicide attempts. These drugs are prescribed to those who struggle with anxiety disorders or insomnia and are highly addictive due to rapidly increased tolerance. While the possibility exists that the insomnia and anxiety are to blame for the suicidal behaviors, several other studies seem to suggest that the drugs themselves were causing the suicide attempts. In addition, these sedatives are often used as a tool to complete a suicide, often combined with alcohol.
Opioid Abuse and Suicide
 The opioid epidemic that has ravaged the nation has focused attention primarily on overdose death rates. One overlooked phenomenon in studying opioid abuse surrounds the high suicide rates among addicts, as many of the deaths were likely not accidental. The risk of suicide among men with an opioid use disorder was two-fold the general population, while among women, there was an eight-fold risk of suicide. Researchers have found that prescription opioid abuse is associated with a 40%-60% increased risk of suicidal ideation.
The opioid epidemic that has ravaged the nation has focused attention primarily on overdose death rates. One overlooked phenomenon in studying opioid abuse surrounds the high suicide rates among addicts, as many of the deaths were likely not accidental. The risk of suicide among men with an opioid use disorder was two-fold the general population, while among women, there was an eight-fold risk of suicide. Researchers have found that prescription opioid abuse is associated with a 40%-60% increased risk of suicidal ideation.
Suicide Prevention Begins with Treatment
 With substance abuse and suicide intrinsically linked, the most effective way to prevent suicide is through a comprehensive addiction treatment program. Completing residential treatment will equip the person with new coping skills acquired through cognitive behavioral therapy, as well as a relapse prevention plan and involvement in the 12-step recovery process. All of these will help the individual in recovery to better manage stressors and to regulate emotions more effectively.
With substance abuse and suicide intrinsically linked, the most effective way to prevent suicide is through a comprehensive addiction treatment program. Completing residential treatment will equip the person with new coping skills acquired through cognitive behavioral therapy, as well as a relapse prevention plan and involvement in the 12-step recovery process. All of these will help the individual in recovery to better manage stressors and to regulate emotions more effectively.
Recognizing the presence of a co-occurring mental health issue is critical for preventing suicidal thoughts and behaviors. A high percentage of individuals who complete suicide had a history of depression and alcoholism or some other drug dependency. Dual diagnosis treatment is designed to help individuals with both a substance use disorder and a mental health disorder to overcome both disorders, thereby improving overall quality of life.
DreamLife Recovery is a residential addiction recovery program located in Donegal, Pennsylvania. Substance abuse is strongly correlated with a significant increase in suicide risk, with or without a co-occurring mental health disorder. If you or a loved one is struggling with addiction and suicidal thoughts, please reach out to our admissions team today at (844) 402-3592.
Resources:
- “Risk Factors and Warning Signs” – American Foundation for Suicide Prevention
- “Does alcohol and other drug abuse increase the risk for suicide?” – U.S. Department of Health and Human Services, Digital Communication Division, Rev. 7 May, 2008
- “Benzodiazepines May Increase Suicide Risk in Some Patients” – Tumolo, Jolynn; Psychiatry & Behavioral Health Learning Network, 17 October, 2018
- “Addressing Two Public Health Epidemics: Suicide and Opioid Addiction” – Pond, Emily; Psychiatry Advisor, 26 November, 2019
- “A Closer Look at Substance Use and Suicide” – Michael Esang, M.B.B.Ch., M.P.H., Saeed Ahmed, M.D.; The American Journal of Psychiatry: Residents’ Journal, 1 June, 2018
- Beck AT, Steer RA. Clinical predictors of eventual suicide: a 5-to 10-year prospective study of suicide attempters. J Affect Disord. 1989 Nov-Dec;17(3):203-9